Mutated corona virus shows significant boost in infectivity

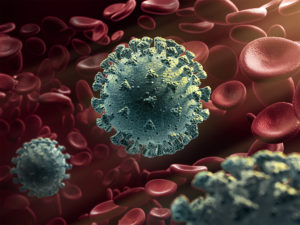
In this cryogenic electron microscope image of a SARS-CoV-2 spike protein side view, the S1 section of the spike is shown in green and the S2 portion is shown in purple. This unique two-piece system has shown itself to be relatively unstable. A new mutation has appeared in the viral variant most common in New York and Italy that makes this spike both more stable and better able to infect cells. (Credit: Andrew Ward lab, Scripps Research)
“COVID-19-causing viral variant taking over in the United States and Europe now carries more functional, cell-binding spikes.”
SOURCE: Scripps Research Institute, Florida
A tiny genetic mutation in the SARS corona virus 2 variant circulating throughout Europe and the United States significantly increases the virus’ ability to infect cells, lab experiments performed at Scripps Research show.
“Viruses with this mutation were much more infectious than those without the mutation in the cell culture system we used,” says Scripps Research virologist Hyeryun Choe, PhD, senior author of the study.
The mutation had the effect of markedly increasing the number of functional spikes on the viral surface, she adds. Those spikes are what allow the virus to bind to and infect cells.
“The number—or density—of functional spikes on the virus is 4 or 5 times greater due to this mutation,” Choe says.
The spikes give the corona virus its crown-like appearance and enable it to latch onto target cell receptors called ACE2. The mutation, called D614G, provides greater flexibility to the spike’s “backbone,” explains co-author Michael Farzan, PhD, co-chairman of the Scripps Research Department of Immunology and Microbiology.
More flexible spikes allow newly made viral particles to navigate the journey from producer cell to target cell fully intact, with less tendency to fall apart prematurely, he explains.
“Our data are very clear, the virus becomes much more stable with the mutation,” Choe says.
There has been much debate about why COVID-19 outbreaks in Italy and New York have so quickly overwhelmed health systems, while early outbreaks in places like San Francisco and Washington state proved more readily managed, at least initially. Was it something about those communities and their response, or had the virus somehow changed?
All viruses acquire minute genetic changes as they reproduce and spread. Those changes rarely impact fitness or ability to compete. The SARS-CoV-2 variant that circulated in the earliest regional outbreaks lacked the D614G mutation now dominating in much of the world.
But was that because of the so-called “founder effect,” seen when a small number of variants fan out into a wide population, by chance? Choe and Farzan believe their biochemical experiments settle the question.
“There have been at least a dozen scientific papers talking about the predominance of this mutation,” Farzan says. “Are we just seeing a ‘founder effect?’ Our data nails it. It is not the founder effect.”
Choe and Farzan’s paper is titled “The D614G mutation in the SARS-CoV-2 spike protein reduces S1 shedding and increases infectivity.” Now undergoing peer review, it is being posted prior to publication to the pre-print site bioRxiv, and released early, amid news reports of its findings.
Choe and Farzan note that their research was performed using harmless viruses engineered to produce key coronavirus proteins. Whether the changes they observed also translate to increased transmissibility in the real world requires additional epidemiological studies, they note.
Encouragingly, the duo found that immune factors from the serum of infected people work equally well against engineered viruses both with and without the D614G mutation. That’s a hopeful sign that vaccine candidates in development will work against variants with or without that mutation, Choe says.
Choe and Farzan have studied coronaviruses for nearly 20 years, since the first outbreak of SARS, a similar virus. They were the first to discover in 2003 that SARS bound to the ACE2 receptor on cells. Others’ experiments have shown the SARS-CoV-2 virus binds the same ACE2 receptor.
But Farzan and Choe note a key structural difference between spike proteins on the first SARS virus and this new pandemic strain. With both, under an electron microscope, the spike has tripod shape, with its three segments bound together at a backbone-like scaffold. But SARS-CoV-2 is different. Its tripod is divided in two discreet segments, S1 and S2.
Initially, this unusual feature produced unstable spikes, Farzan says. Only about a quarter of the hundreds of spikes on each SARS-CoV-2 virus maintain the structure they need to successfully infect a target cell. With the mutation, the tripod breaks much less frequently, meaning more of its spikes are fully functional, he says.
The addition of the D614G mutation means that the amino acid at that location is switched from aspartic acid to glycine. That renders it more bendable, Farzan says. Evidence of its success can be seen in the sequenced strains that scientists globally are contributing to databases including GenBank, the duo reports. In February, no sequences deposited to the GenBank database showed the D614G mutation. But by March, it appeared in 1 out of 4 samples. In May, it appeared in 70 percent of samples, Farzan says.
“Over time, it has figured out how to hold on better and not fall apart until it needs to,” Farzan says. “The virus has, under selection pressure, made itself more stable.”
It is still unknown whether this small mutation affects the severity of symptoms of infected people, or increases mortality, the scientists say. While ICU data from New York and elsewhere reports a preponderance of the new D614G variant, much more data, ideally under controlled studies, are needed, Choe says.
In addition to senior authors Choe and Farzan, the authors include first authors Lizhou Zhang, Cody Jackson and Huihui Mou, plus co-authors Amrita Ojha, Erumbi Rangarajan and Tina Izard, all of Scripps Research.
The work was supported by the National Institutes of Health through an administrative supplement to RO1 AI129868 for coronavirus research.
- New, more infectious strain of Covid-19 now dominates global cases of virus - July 14, 2020
- COVID-19 threatens the entire nervous system - June 22, 2020
- Mutated corona virus shows significant boost in infectivity - June 14, 2020